What do the 7 Stages of Alzheimer’s disease mean?
As a “slowly progressive” illness, Alzheimer’s disease has a likely* set of symptoms that appear over several years. The likely progression of symptoms and the likely time frame has been put into the FAST Scale (aka FAST Stage). FAST stands for Functional Assessment Staging Tool.
*Experts use the term “likely” when referring to the stages, rate of progression, and symptoms. In Alzheimer’s disease there is considerable variation from person to person and stage to stage. Some people’s illness progresses more rapidly or more slowly than expected. Some people have one or two symptoms of a more advanced stage, but not all.
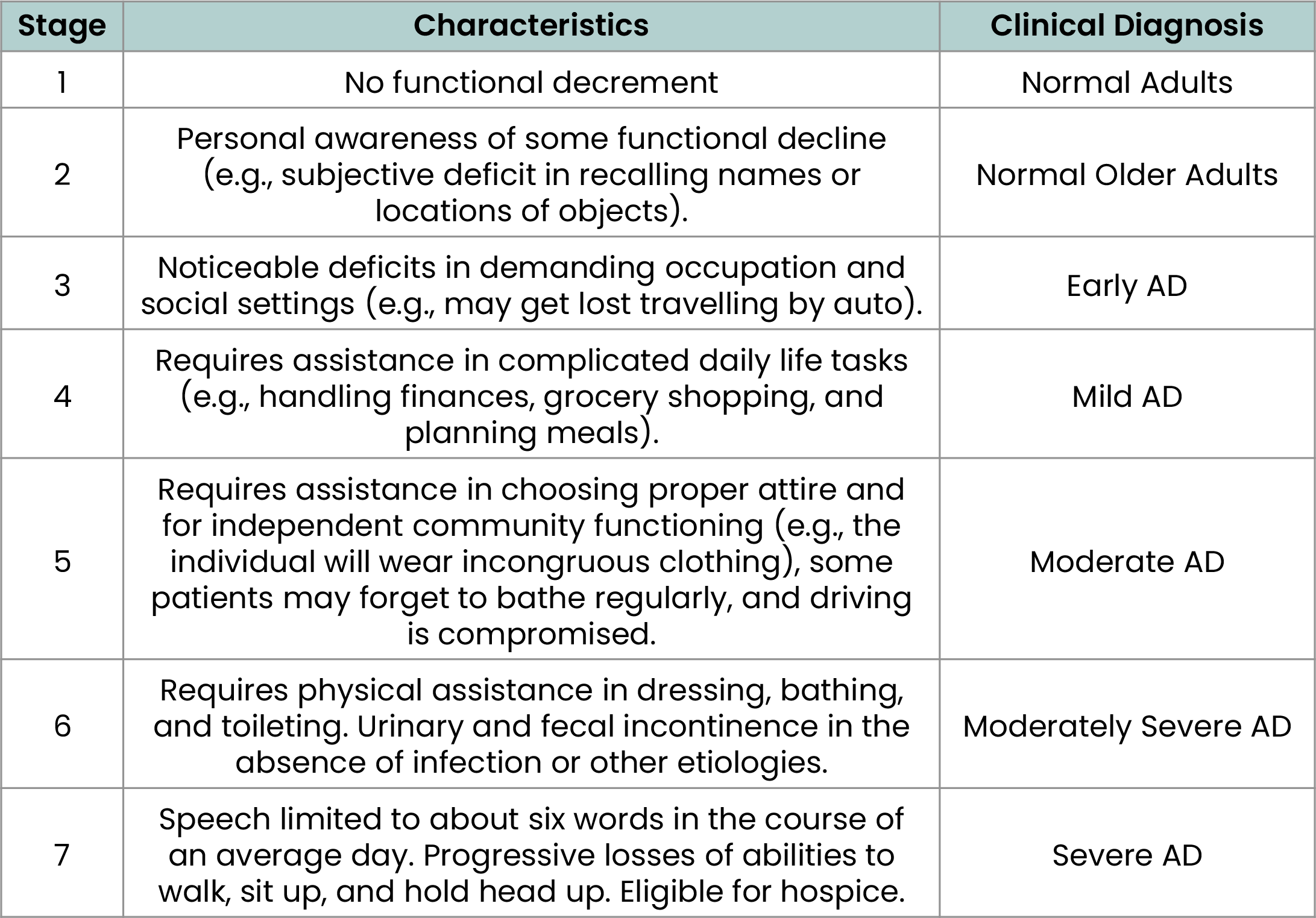
FAST Stages
There is a number and descriptor for each of the 7 stages of illness.
Stage 1 and 2 signifies normal aging.
Stage 3/Early Stage begins at diagnosis and typically lasts 3-5 years.
Stage 4/Mild Stage typically lasts up to 5 years.
Stage 5 and Stage 6/Moderate Stage can last up to 5-10 years.
Stage 7/Severe Stage lasts 1-2 years.
Notice that the FAST scale is a “functional assessment”. This highlights the difficult reality of how Alzheimer’s disease affects the brain and changes those affected. As it begins in an area of the brain dedicated to memory, where it changes an individual’s ability to make a new memory. That in turn, impacts your loved one’s ability to do other functions as they relate to memory. For example, your loved one may lose items, forget appointments, skip medication doses, etc.
As Alzheimer’s disease progresses and its effects damage additional parts of the brain, the functions associated with those areas begin to change as well. Early stages are primarily intellectual functions for example memory, or concentration. Later stages begin to include functions of a more physical nature -- for example unsteadiness walking or difficulty swallowing.
How are the Stages of Alzheimer’s Disease Determined?
When we want to determine an individual’s stage of illness, family caregivers often think it is some aspect of cognitive testing or a physical finding on a brain scan. In Alzheimer’s, however, there is no such testing available. Rather it is the functional abilities of an individual that identifies their stage of the disease. Those functional abilities are seen in the day-to-day array of life activities (shopping, paying bills, planning meals, managing medical care) and personal care (dressing, personal hygiene, exercise/activities). For example, an individual in Early Stage will have little trouble doing everything they need to do every day, including even complicated life tasks such as shopping or planning meals. In the Mild Stage, that same individual will need some help with those activities but will still be able to participate in that activity. By the Moderate Stage many individuals will no longer be able to shop or do meal planning without the full support of a family caregiver.
How Does Knowing the Stage of My Loved One’s Illness Help Family Caregivers?
There are 2 ways “knowing the stage” helps you and your loved one.
First, the stages identify the likely cognitive deficits and functional difficulties your loved one will face. Knowing this, Family Caregivers can focus their efforts on targeted strategies that make up for the cognitive decline, and allow for as much success and independence as possible.
For example, if you know your loved one is in Stage 4/Mild Alzheimer’s Disease, you will understand that but your loved one is likely to be able to manage a shopping trip on their own, with Family Caregivers needed only as “back-up” or on “stand-by” assistance. Having your loved one create a shopping list, and reviewing it just before they head to the store, will increase their chances of success.
On the other hand, if your loved one is in Stage 5/Moderate Alzheimer’s Disease, it is less likely your loved one will be successful shopping on their own. It’s likely best for you to shop together. In addition, you will learn that most individuals in Stage 5 have reduced ability to stay safe while driving by themselves. For that reason, too, sharing the shopping responsibilities is likely best.
Second, the stages identify the likely issues and changes that are coming, so that Caregivers can educate themselves and prepare as needed.
Developed at the New York University Medical Center’s Aging and Dementia Research Center, the Functional Assessment Staging (FAST) Scale provides a method of staging AD for initial and ongoing assessment
Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139(9):1136-1139.